Understanding Plantar Fasciitis
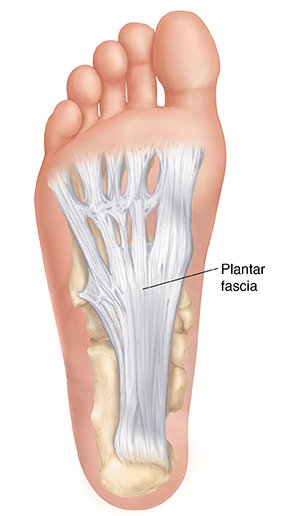
Plantar fasciitis is a condition that causes foot and heel pain. The plantar fascia is a tough band of tissue that runs across the bottom of the foot from the heel to the toes. This tissue pulls on the heel bone. It supports the arch of the foot as it pushes off the ground. If the tissue becomes irritated or red and swollen (inflamed), it's called plantar fasciitis.
How to say it
PLAN-tar fa-shee-I-tihs
What causes plantar fasciitis?
Plantar fasciitis most often occurs from overusing the plantar fascia. The tissue may become damaged from activities that put repeated stress on the heel and foot. Or it may wear down over time with age and ankle stiffness. You're more likely to have plantar fasciitis if you:
-
Do activities that require a lot of running, jumping, or dancing
-
Have new or increased activity
-
Have a job that requires being on your feet for long periods
-
Are overweight or obese
-
Have certain foot problems, such as a tight Achilles tendon, flat feet, or high arches
-
Often wear poorly fitting shoes
Symptoms of plantar fasciitis
The condition most often causes pain in the heel and the bottom of the foot. The pain may occur when you take your first steps in the morning. It may get better as you walk during the day. But as you continue to put weight on the foot, the pain often returns. Pain may also occur after standing or sitting for long periods.
Treating plantar fasciitis
Treatments for plantar fasciitis include:
-
Resting the foot. This includes limiting movements that make your foot hurt. You may also need to not do certain sports and types of work for a time.
-
Using cold packs. Put an ice pack on the heel and foot to help reduce pain and swelling. To make an ice pack, put ice cubes in a plastic bag that seals at the top. Wrap the bag in a thin towel or cloth. Don’t put ice or an ice pack directly on the skin.
-
Taking medicines. Prescription and over-the-counter medicines can help ease pain and swelling. NSAIDs (nonsteroidal anti-inflammatory drugs) are the most common medicines used. They may be given as pills. Or they may be put on the skin as a gel, cream, or patch.
-
Using heel cups or foot inserts (orthotics). These are placed in the shoes to help support the heel or arch and cushion the heel. You may also be advised to buy correct-fitting shoes with good arch support and cushioned soles.
-
Taping the foot. This supports the arch and limits the movement of the plantar fascia to help ease symptoms.
-
Wearing a night splint. This stretches the plantar fascia and leg muscles while you sleep. This may help ease pain.
-
Doing exercises and physical therapy. These stretch and strengthen the plantar fascia and the muscles in the leg that support the heel and foot. Stretching your calf and plantar fascia is the most effective way to ease pain.
-
Getting shots of medicine into the foot. These may help ease symptoms for a time. The shots often contain corticosteroids. These are strong anti-inflammatory medicines.
-
Having surgery. This may be needed if other treatments don't ease symptoms. During surgery, the surgeon may partially cut the plantar fascia to release tension.
Possible complications of plantar fasciitis
Without correct care and treatment, healing may take longer than normal. Also, symptoms may continue or get worse. Over time, the plantar fascia may be damaged. This can make it hard to walk or even stand without pain.
When to call your healthcare provider
Call your healthcare provider right away if you have any of these:
-
Fever of 100.4°F (38°C) or higher, or as advised by your provider
-
Chills
-
Symptoms that don’t get better with treatment, or get worse
-
New symptoms, such as numbness, tingling, or weakness in the foot